The most appropriate response is to lower this women's blood pressure immediately using intravenous agents. Normally this would include a ß-blocking agent to lower blood pressure, heart rate and dp/dt, all of which are thought to promote extension of the aortic dissection. A second drug, frequently a vasodilating agent, is then added to the ß-blocker. An excellent single agent would be Labetalol with both alpha- and beta- properties. The key is not only to lower the arterial pressure to as low as tolerated but to also prevent the reflex tachycardia which would increase shear stresses on the aortic root.
Transthoracic echocardiography is relatively insensitive (31-55%) for picking up distal aortic dissection and 78-100% for ascending dissection, but still less sensitive than a transesophageal echocardiographic study (TEE). Therefore most prefer computed tomographic scanning or the TEE in making the intial diagnosis of aortic dissection. There are some recent studies that seem to point to MRI as being the best test if the patient can be medically stabilized. The major downfall to the MRI is the fact that the patient needs to be in the scanner for a long period of time (i.e. 30-60 minutes).
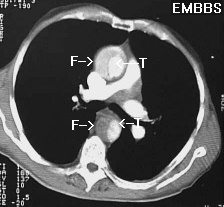
This particular patient got a CT scan which showed the following:
F=false lumen; T=true lumen
Calling a cardiovascular surgeon is the next priority while one is lowering the blood pressure and arranged for the appropriate thoracic imaging study. Favorable signs in this patient include no clinical signs of aortic insufficiency, carotid or arm pulse deficit, or a neurologic syndrome. She is exhibiting anterior chest pain which suggests possible involvement of the ascending aorta. The fact that she found no relief with nitroglycerin and a normal EKG should make aortic dissection a STRONG consideration.
Ordering spinal radiographs addresses the possibility that a ruptured vertebral disc has caused such severe pain that the patient's hypertension was related to this instead. Though this is conceivable we must rule out potentially life-threatening conditions first. Further work-up of less threatening possibilites can then follow.
An abdominal aortic aneurysm rupture is plausible, several features make this less desirable than urgent lowering of blood pressure. First, there is no history of pre-existing aortic aneurysm. Second, the pain is in the back, not in the flanks. Third, this patient presented with hypertension and a normal abdominal examination. Ordinarily, a ruptured abdominal aortic aneurysm is accompanied by abdominal tenderness and/or quiet bowel sounds and frequently hypotension is present.
Various underlying etiologies for aortic dissection include:
NOTE: syphilis is NOT a cause of aortic dissection and in fact due to scarring in the proximal aorta may infact partially protect a patient from suffering this often fatal disease.
Also do not forget that the biggest predictor of having an aortic dissection is prior history of one. Said another way, the recurrence rate for aortic dissection is high and a person with this diagnosis needs careful life-long monitoring of their blood pressure.
References: