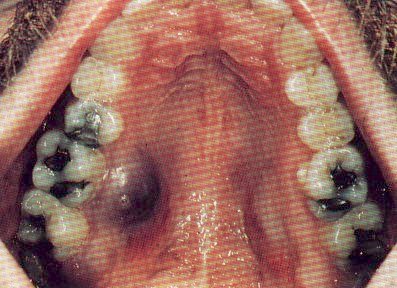
Recognizing the multiple oral manifestations of HIV infection are important clues that may lead you to suspect HIV/AIDS in a first time visiting patient. Often times a previously asymptomatic patient may walk into your office or clinic with the above findings. It then becomes incumbent on you as a physician to identify the underlying immunodeficiency state. In these days, the most important underlying immunocomprised state to identify is HIV/AIDS.
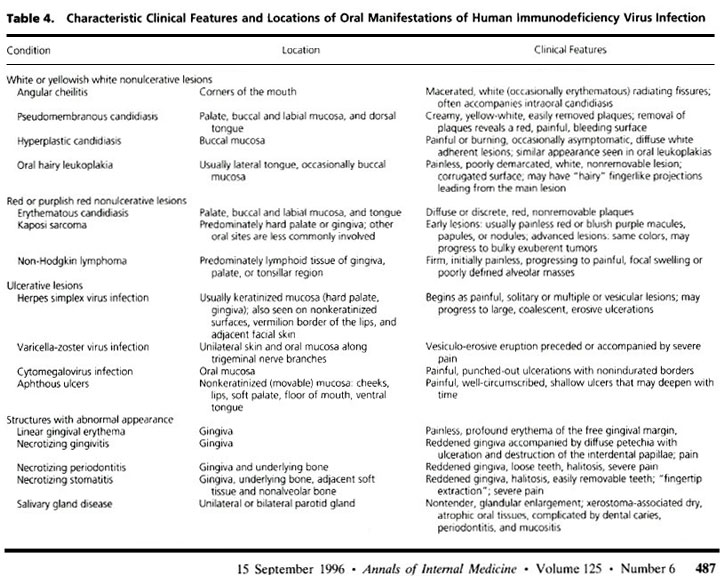
This patient has already been identified as an HIV/AIDS patients who is receiving "the three drug cocktail" therapy. This removable exudate is, of course, thrush. Often times a patient who is dehydrated or has had decreased oral intake may have a "coated" tongue. Clinically, you can differentiate the two by being able to scrape off the Candida with a tongue blade, often times leaving a bloody, painful denudation mark.
As to how to treat this patient there are really two appropriate answers, though one might be better than the other based on the severity of related symptoms. For instance, if this episode of thrush is caught early and has had minimal effects on a patients nutritional intake one could treat with oral mycelex troches. This is preferred since fungal Diflucan resistance can be promoted if one uses this agent repetitively. As such, one would like to save this for a possible future need. However, if the thrush is associated with severe odynophagia, dysphagia and decreased oral intake a short course of Diflucan can help rapidly get the Candida esophagitis under control. Another good candidate for Diflucan would be a patient with repetitive, severe episodes only responsive to Diflucan in the past.
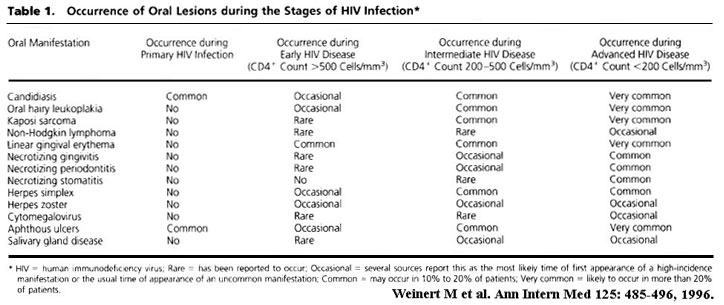
The following tables (1) provide a good listing of the many possible oral lesions identified in the mouth of HIV/AIDS patients:
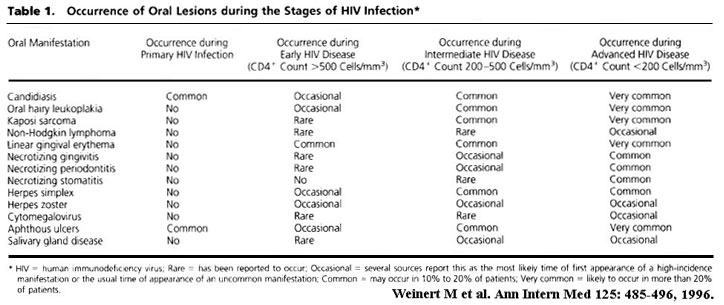
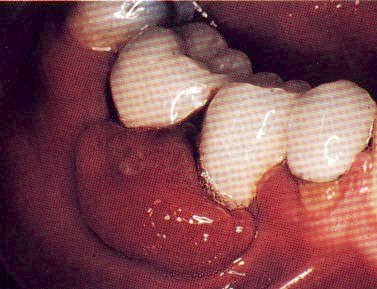
Other lesions important to identify include the following:
These have most recently been to be responsive to Thalidomide (2).

This is treated with Acyclovir.
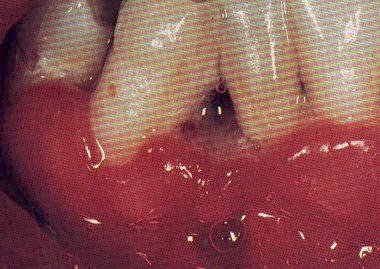
Which will require biopsy proof before the institution of chemotherapy.
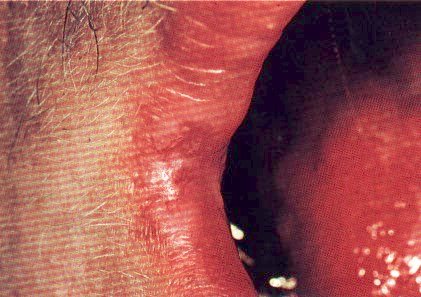
This is felt to be secondary to EBV infection and may respond to Acyclovir as well.

This obviously needs a tissue biopsy for confirmation. Lymphoma in AIDS patients typically presents with CNS involvement and portrends a poor prognosis with most patients dead within 6 months despite chemotherapy.
This is important to recognize and when seen you might suspect the patient has DILS (Diffuse Infiltrative Lymphocytosis Syndrome) i.e. Sjogren's Syndrome in AIDS.
Finally, this condition is frequently seen and is caused typically by Candida. It is an early sign of thrush in that when a patient sleeps some of his/her saliva will pool in the angle of the mouth and cause a Candida chelitis. You would treat this with a topical antifungal cream/ointment unless obvious thrush is found in the oral cavity.
References: