Bone Marrow Embolus
Bone Marrow Embolus
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Congested liver, dead cells in zone 3
Congested liver, dead cells in zone 3
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Great fibrin cap
Great fibrin cap
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Heart Failure Cells
Heart Failure Cells
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Hyalinized intramyocardial artery (diabetes)
Hyalinized intramyocardial artery (diabetes)
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Congested liver, live cells in zone 1
Congested liver, live cells in zone 1
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Intrapulmonary hemorrhage
Intrapulmonary hemorrhage
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Myocardium
Myocardium
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Nodular diabetic glomerulosclerosis
Nodular diabetic glomerulosclerosis
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Myocardial ischemic scar
Myocardial ischemic scar
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
 Subendocardial ischemic scar
Subendocardial ischemic scar
Slide from Andrea McCollum MD
Cuyahoga County Coroner's Office
BLOOD VESSELS
Ed Friedlander, M.D., Pathologist
scalpel_blade@yahoo.com


Cyberfriends: The help you're looking for is probably here.
Welcome to Ed's Pathology Notes, placed
here originally for the convenience of medical students
at my school. You need to check the accuracy of any
information, from any source, against other credible
sources. I cannot diagnose or treat over the web,
I cannot comment on the health care you have already
received,
and these notes cannot substitute for your
own doctor's care. I am good at helping people find
resources and answers. If you need me, send me an
E-mail at scalpel_blade@yahoo.com Your confidentiality is completely respected.
 DoctorGeorge.com is a larger, full-time service.
There is also a fee site at myphysicians.com,
and another at www.afraidtoask.com.
DoctorGeorge.com is a larger, full-time service.
There is also a fee site at myphysicians.com,
and another at www.afraidtoask.com.
Translate this page automatically
 |
With one of four large boxes of "Pathguy" replies. |
 I'm still doing my best to answer
everybody.
Sometimes I get backlogged,
sometimes my E-mail crashes, and sometimes my
literature search software crashes. If you've not heard
from me in a week, post me again. I send my most
challenging questions to the medical student pathology
interest group, minus the name, but with your E-mail
where you can receive a reply.
I'm still doing my best to answer
everybody.
Sometimes I get backlogged,
sometimes my E-mail crashes, and sometimes my
literature search software crashes. If you've not heard
from me in a week, post me again. I send my most
challenging questions to the medical student pathology
interest group, minus the name, but with your E-mail
where you can receive a reply.
Numbers in {curly braces} are from the magnificent
Slice
of Life videodisk. No medical student should
be without access to this wonderful resource.
Someday you may be able to access these
pictures directly from this page.
 I am presently adding clickable links to
images in these notes. Let me know about good online
sources in addition to these:
I am presently adding clickable links to
images in these notes. Let me know about good online
sources in addition to these:
Also:
Medmark Pathology -- massive listing of pathology sites
Pathology Handout -- Korean student-generated site; I am pleased to permit their use of my cartoons
Estimating the Time of Death -- computer program right on a webpage
Pathology Field Guide -- recognizing anatomic lesions, no pictures

Freely have you received, freely give. -- Matthew 10:8. My
site receives an enormous amount of traffic, and I'm
handling about 200 requests for information weekly, all
as a public service.
Pathology's modern founder,
Rudolf
Virchow M.D., left a legacy
of realism and social conscience for the discipline. I am
a mainstream Christian, a man of science, and a proponent of
common sense and common kindness. I am an outspoken enemy
of all the make-believe and bunk that interfere with
peoples' health, reasonable freedom, and happiness. I
talk and write straight, and without apology.
Throughout these notes, I am speaking only
for myself, and not for any employer, organization,
or associate.
Special thanks to my friend and colleague,
Charles Wheeler M.D.,
pathologist and former Kansas City mayor. Thanks also
to the real Patch
Adams M.D., who wrote me encouragement when we were both
beginning our unusual medical careers.
If you're a private individual who's
enjoyed this site, and want to say, "Thank you, Ed!", then
what I'd like best is a contribution to the Episcopalian home for
abandoned, neglected, and abused kids in Nevada:
I've spent time there and they are good. Write "Thanks
Ed" on your check.

My home page
More of my notes
My medical students
Especially if you're looking for
information on a disease with a name
that you know, here are a couple of
great places for you to go right now
and use Medline, which will
allow you to find every relevant
current scientific publication.
You owe it to yourself to learn to
use this invaluable internet resource.
Not only will you find some information
immediately, but you'll have references
to journal articles that you can obtain
by interlibrary loan, plus the names of
the world's foremost experts and their
institutions.
Alternative (complementary) medicine has made real progress since my
generally-unfavorable 1983 review linked below. If you are
interested in complementary medicine, then I would urge you
to visit my new
Alternative Medicine page.
If you are looking for something on complementary
medicine, please go first to
the American
Association of Naturopathic Physicians.
And for your enjoyment... here are some of my old pathology
exams
for medical school undergraduates.
I cannot examine every claim that my correspondents
share with me. Sometimes the independent thinkers
prove to be correct, and paradigms shift as a result.
You also know that extraordinary claims require
extraordinary evidence. When a discovery proves to
square with the observable world, scientists make
reputations by confirming it, and corporations
are soon making profits from it. When a
decades-old claim by a "persecuted genius"
finds no acceptance from mainstream science,
it probably failed some basic experimental tests designed
to eliminate self-deception. If you ask me about
something like this, I will simply invite you to
do some tests yourself, perhaps as a high-school
science project. Who knows? Perhaps
it'll be you who makes the next great discovery!
Our world is full of people who have found peace, fulfillment, and friendship
by suspending their own reasoning and
simply accepting a single authority that seems wise and good.
I've learned that they leave the movements when, and only when, they
discover they have been maliciously deceived.
In the meantime, nothing that I can say or do will
convince such people that I am a decent human being. I no longer
answer my crank mail.
This site is my hobby, and I presently have no sponsor.
This page was last updated February 6, 2006.
During the ten years my site has been online, it's proved to be
one of the most popular of all internet sites for undergraduate
physician and allied-health education. It is so well-known
that I'm not worried about borrowers.
I never refuse requests from colleagues for permission to
adapt or duplicate it for their own courses... and many do.
So, fellow-teachers,
help yourselves. Don't sell it for a profit, don't use it for a bad purpose,
and at some time in your course, mention me as author and KCUMB as my institution. Drop me a note about
your successes. And special
thanks to everyone who's helped and encouraged me, and especially the
people at KCUMB
for making it possible, and my teaching assistants over the years.
Whatever you're looking for on the web, I hope you find it,
here or elsewhere. Health and friendship!


More of Ed's Notes:


I [Allah] am nearer to you than the vein in your neck. --Koran
QUIZBANK:
Hemodynamic #'s 1-30,
Vessels (all)
Atherosclerosis: Hemodynamic 1-30
Tumors / Aneurysms / Vasculitis: Vessels (all)
Learn First
The term "arteriosclerosis" (literally, "hardening of the arteries") should be avoided by physicians.
It includes (1) atherosclerosis; (2) Monckeberg's medial calcific sclerosis; and (3) arteriolar sclerosis
(hyaline, hyperplastic, intimal fibrosis). Unqualified, the term usually means "atherosclerosis".
The vascular intima looks simple but isn't. Endothelial cells must maintain their no-stick inner
surfaces, help constrict and dilate vessels, and heal damaged vessels. Myointimal cells and
macrophages, located between the endothelium and the internal elastic membrane, are the principal
actors in atherosclerosis.
Atherosclerosis is a stereotyped response of the inner surfaces of large arteries to a variety of insults.
In this disease, the cells between the endothelium and the internal elastic membrane take up
cholesterol-rich lipid, which then causes harm. Lesions progress from fatty steaks to fibrous plaques
to complicated fibrous plaques; they can also regress.
Atherosclerosis may calcify, but the problem in atherosclerosis is not the dystrophic calcification.
Monckeberg's medial calcific sclerosis just means dystrophic
calcification of the media of an artery, but it
is almost never a real problem.
Atherosclerosis was the great killer of 20th century North Americans. The epidemic
peaked in 1968, and since then the decline has been spectacular, due more than anything else to
healthier lifestyles (JAMA 277: 535, 1997; it's
been steady since the mid-1980's: NEJM 339: 861, 1998).
We are beginning to understand how the common risk
factors relate to its pathogenesis. Americans are taking steps to protect themselves, and lifestyle
changes can almost certainly reverse much of the damage in all but the most advanced lesions.
Hyaline arteriolar sclerosis results from damage to arterioles usually from
increased pressure or increased blood glucose.
Hyperplastic arteriolar sclerosis involves hyperplasia of the intimal cells; it
results from processes that do severe, acute damage to the endothelium.
Fibrosis of the intima results from high blood pressure or "just getting older."
 OBJECTIVES: This is mastery material.
OBJECTIVES: This is mastery material.
Give a full account of atherosclerosis, its causes and effects,
its full range of anatomic pathology, and its complications.
Make sense of its risk factors in terms of what we know
about its chemistry and pathophysiology.
Recognize each of these anatomic lesions, grossly and/or microscopically as applicable:
atheroembolization
atherosclerotic aneurysm
fatty streak
fibrous plaque
hemorrhage into an atherosclerotic plaque
ulcerated atherosclerotic plaque
Give a full account of the vascular changes contributing
to, and resulting from, high blood pressure.
Give a full account of each of these clinical syndromes, with anatomic
and clinical pathology as applicable:
arteriovenous malformation
Buerger's thromboangiitis obliterans
Churg-Strauss disease
Kawasaki mucocutaneous lymph node syndrome
leukocytoclastic vasculitis
Takayasu's pulseless disease
temporal arteritis
varicose veins
Wegener's granulomatosis
Describe the range of infections that can affect the blood vessels.
Review the causes of deep vein thrombosis ("thrombophlebitis"),
and describe its symptoms, signs, and principal complication.
Give accounts
of each of the following, and be able to recognize them clinically:
inferior vena cava syndrome
lymphangitis
lymphedema
superior vena cava syndrome
Recognize each of these anatomic lesions, grossly and/or microscopically as applicable:
aortic dissection
berry aneurysm
cystic medial necrosis
hyaline arteriolar sclerosis
intimal fibrosis
medial calcific sclerosis
syphilitic aneurysm
Weibel-Palade body
Describe the important tumors, hamartomas, and proliferations
of blood and lymph vessels,
how they behave clinically, and the pitfalls in making the diagnosis.
 NORMAL ANATOMY
NORMAL ANATOMY
Arteries carry blood from the heart.
Elastic arteries ("large arteries") include the aorta and at least the beginnings of its largest branches.
These arteries both propel and dampen the pulse wave. These are distinguished by a preponderance
of elastic fibers in their media. The subendothelium of their intimal layers thickens over the course
of life through the accumulation of collagen fibers and myointimal cell. The elastic tissue
proliferates here. You already know that all elastic tissue slowly
breaks down as we age. In older adults,
the elastic is largely replaced by collagen. This also results in lengthening and thus tortuosity seen
in older people. The adventitia and outer media is nourished by vasa vasora. All arteries depend
on the blood within their lumens to nourish their intima and inner media.
Muscular arteries ("medium-sized arteries", "distributing arteries") exhibit smooth muscle in their
walls, and may expand and contract to regulate the caliber of the lumen and thus the flow of blood.
The intima is similar to that of the elastic arteries, and it thickens similarly. Smooth muscle may
pass into the intima through fenestrae in the internal elastic membrane. These fenestrae may become
wide in old age and be mistaken for damage from previous vasculitis. The media is bounded on
either side by an inner and outer elastic membrane.
Small arteries are the major site of autonomic regulation of blood flow, and take the worst beating
in hypertension. A rule of thumb is that the wall and lumen should have the same thickness.
Thickening of the intima occurs here as well. In sites of inflammation or tumor, it may be quite
impressive (* "Friedlander's endarteritis obliterans", discovered by the real Dr. Friedlander, 19th
century pathologist Carl, 1847-1887). Hyaline arteriolar sclerosis becomes a problem as we age, especially if
we get diabetes or hypertension. There's no outer elastic membrane, and the layers become
progressively less distinct as the arteries get smaller.
Arterioles continue the anatomy of the small arteries. Two definitions that have been offered:
(1) Arterioles have five or fewer layers of smooth muscle; (2) Arterioles have total diameter
100 microns or
less.
Veins and lymphatics have histologic features that you know.
In disease, veins do not usually show so
much intimal proliferation and fibrosis as do arteries. The muscle in the wall of a vein is thinner,
and in the larger veins tends to be less organized. Very large veins have some layers of elastic
outside their muscular layer. Lymphatics run very close to arteries (even closer than the veins), and
tend to be small and to have thinner walls than the vein that runs with that artery. It's not always
possible to tell lymphatics from veins; if the vessel contains red cells, it's most likely a vein.
Endothelium is special stuff. It is permeable to water and the small inorganic ions. It transports a
little bit of blood protein by pinocytosis. Electron microscopists recognize it by the
Weibel-Palade
bodies (puh-LAH-dee, made of von Willebrand's factor). It can contract, to regulate capillary
flow. It produces some of the subendothelial connective tissue.
It also makes substances: (1) Prostacyclin (to keep its surface slippery); (2) Von Willebrand's factor;
(3) Endothelin (a vasoconstrictor peptide); (4) Endothelial-derived relaxation factor (nitric oxide,
EDRF; see Nature 368: 62, 1994).
Vascular smooth muscle is also special. It has LDL receptors. It can get into the intima through
holes in the internal elastic membrane. Both facts will become important when we study
atherogenesis.
 BIRTH DEFECTS INVOLVING VESSELS
BIRTH DEFECTS INVOLVING VESSELS
There are many variations on the normal anatomy of arteries.
Malformations of the coronary arteries may first announce themselves
by causing sudden death. More about this soon.
The familiar red "birthmarks" are hemangiomas, and will be covered with
"tumors".
The only other
birth defects worth
mentioning are berry aneurysms and arteriovenous malformations ("AV malformations", "AV
fistulas", "AV aneurysms", etc.)
AV malformations involve a tangle of abnormal medium-sized
vessels connecting a large artery and a large vein.
The problem is shunting of the blood away from the territory that should be supplied by the artery.
The vein will tend to expand ("aneurysm").
Sometimes the AV malformation is a mass of wormy vessels ("cirsoid aneurysm", "racemose
aneurysm"; apparently endemic among Klingons). This is most common in the brain, where
subarachnoid hemorrhage is the dread complication.
Future pathologists: It's good to be able to distinguish an baby's AV malformation (which won't go away)
from a baby's hemangioma (which probably will go away),
An AV malformation does not stain for WT1; a hemangioma that will involute does stain for WT1
(Arch. Derm. 141: 1297, 2005).
ATHEROSCLEROSIS (review still good Am. J. Card. 70: 3, 1992; DeBakey
tries to sort out what puts you at risk for what Am. J. Card. 85: 1045, 2000)

{03476} coronary artery atherosclerosis
{06485} coronary artery atherosclerosis, mild
{06491} coronary artery atherosclerosis, severe
{06497} coronary artery atherosclerosis, total
{09440} atherosclerosis of vertebral and basilar arteries
{09446} êtat cribilé from multiple atheroemboli
Probably still the #1 killer of Americans.
Atherosclerosis causes harm by (1) occluding arteries slowly over time (angina, ischemic scarring of
the myocardium, atherosclerotic dementia, leg claudication, intestinal angina); (2) occluding arteries
suddenly by rupture of plaques (thrombosis, atheroembolization) or hemorrhages into plaques
(myocardial infarct, atherosclerotic stroke, gangrene of the bowel); (3) weakening the walls of
arteries (atherosclerotic aneurysms, penetrating atherosclerotic ulcers of the aorta).
Claudication is the least subtle of these. Patients will have calf pain
after walking a certain distance (usually about the same each time);
the stenosis will of course be way proximal from the pain. Review
Lancet 358: 1257, 2001.
* The radiologists are now able to see a fresh rupture of a fibrous
cap, and correlating it with clinical findings: Circulation 105:
181, 2002; ultrasonography shows that, not surprisingly, the most common site
is at the origin of the LAD (J. Am. Coll. Card. 46: 261, 2005).
{06737} atherosclerosis has caused ischemic fibrosis of the heart
{09443} atherosclerosis of middle cerebral artery
{10889} atheroembolus
 Kidney
Kidney
ERF/KCUMB
You're already familiar with atheroembolization, which is a major cause both of stroke and of lower-extremity ischemia ("blue
toes disease").
Atherosclerosis is a stereotyped response to injury featuring the accumulation of cholesterol-rich fat
in the intima of the large and medium-sized arteries of the body. Typically these are phagocytes
("myointimal cells", visiting macrophages). These masses form plaques, or atheromas.
* Philologists: "Atheros" means "gruel", "porridge", or "grits"; you ate that stuff as Malt-o-Meal.
Think about blobs of 7-day-old dried buttery
Malt-o-Meal lining a dirty sink, and you have a pretty good
idea about atherosclerosis.
For whatever reason, these cells have a great appetite for LDL cholesterol. When the LDL is
abnormal (Ox-LDL, lipoprotein A; see below), or the LDL is processed down the "bad"
(non-apoprotein B receptor-mediated)
breakdown pathway, these cells accumulate lipid that damages
them and their neighbors. The two pathways: Proc. Nat. Acad. Sci. 91: 4431, 1994.
A good working rule: The pulmonary arteries do not get serious
atherosclerosis. Otherwise, if an artery has its own name, it can be significantly affected by
atherosclerosis. The aortic surfaces of the aortic valve cusps are also prone
to the disease at all stages (Heart 91: 576, 2005 documents what all pathologists already knew).
Atherosclerosis seems to be the stereotyped way in which most of the large named arteries respond to
a variety of injuries. Don't expect a unified theory of atherogenesis yet. However,
the manageable risk factors
are, in descending order (1-5 at least) of importance:
1. High levels of LDL cholesterol. This is the over-riding risk factor. Review Lancet 345: 362,
1995.
Your LDL level is a reflection of your heredity, your diet (cholesterol-rich
diets raise LDL), and your exercise habits.
Also remember cholestatic jaundice, nephrotic syndrome, hypothyroidism (* you need T3
to express LDL receptors on liver cells), amiodarone (* keeps T3 from
letting you make LDL receptors) and (less striking)
Cushingism.
As total cholesterol rises above 160 mg/dL, coronary risk rises roughly linearly.
* The Swedish simvastatin study, which laid to rest concerns about excess mortality from lowering
LDL's: 345: 1274, 1995.
2. Cigaret smoking, "which damages the intima".
* "Cigaret" is the preferred spelling. The suffix "-ette" makes the practice sound cute and harmless.
The old story about tobacco "damaging the intima" is giving way to the better-evidenced fact that
tobacco smoke oxidizes LDL, making them into the poorly-digested form that accumulates in the
intima.
This is for me still the most interesting work in atherosclerosis. Oxidized LDL is chemotactic for
macrophages, makes them proliferate, and is cytotoxic once they ingest it, it can make cells produce
cytokines like α-TNF that may be fibrogenic, and it
there can even be autoantibodies.
Smoking oxidizes LDL, HDL protects it from oxidation, vitamin E prevents LDL oxidation (kind
of, antioxidants seem to slow atherosclerosis JAMA 273: 1899, 1995), and so forth and so forth.
* Update on Ox-LDL in atherogenesis: J. Am. Coll. Card. 43:
1731, 2004.
Pathologists: J. Clin. Inv. 92: 471, 1993.
Superoxide plus
NO. generates the noxious ONOO- peroxynitrite radical that oxidizes LDL (Proc. Nat. Acad. Sci.
91: 1044, 1994).
* A variety of other modifications of LDL also result in increased phagocytosis by macrophages,
render it toxic to endothelium, smooth muscle, and macrophages, etc., etc.
3. High blood pressure "which damages the intima". Review Lancet 345: 362, 1995.
Angiotensin II itself is now one of the "usual suspects"
in discussions of molecules that mediate atherogenesis: Am. J. Med. Sci. 323:
17, 2002.
4. Diabetes from any cause.
You'll read a tremendous amount about different effects of hyperglycemia,
insulin,
and so forth on
lipoproteins (Diabetes 41 S 2: 102, 1992), protein chemistry, and so forth. The most interesting
work right now (Science 258: 651, 1992) focuses on advanced glycosylation end-products
("glycation products"), proteins
that have been non-enzymatically glycosylated (* Schiff-base --> Amadori product --> durable
fluorescent product). Binding of these to endothelium makes it permeable, they inactivate nitric
oxide, there are receptors for these substances which, when they bind, cause
cells to produce fibrous tissue, glycosylated LDL probably can't be
processed normally, etc., etc.
Once advanced glycation products have accumulated on board, runaway atherosclerosis
affects even diabetics who have been restored to euglycemia.
Exciting news: Giving the soluble form of the glycation product
receptor removes the products and suppresses accelerated atherosclerosis.
See Nat. Med. 4: 1025, 1998.
* Another idea: High blood glucose levels cause overexpression of CD36,
the LDL scavenger pathway receptor: Nat. Med. 7: 840, 2001.
 5.
Lack of exercise (made "official" in 1992), independent of the above (NEJM
330: 1565, 1992).
5.
Lack of exercise (made "official" in 1992), independent of the above (NEJM
330: 1565, 1992).
The effects of physical exercise are numerous. Possibly "getting in shape" changes lipoprotein
receptor counts, etc., etc. However, contrary to popular mythology, people who are very physically
fit can and do still get serious atherosclerosis.
* Couch potatoes wishing to increase the numbers of LDL-receptors
without exercising may benefit from a new class of drugs that
bind to the sterol regulatory element-binding
protein cleavage-activating protein (Nature Med. 7: 1332, 2001).
In the meantime, exercise capacity actually seems to be the best
predictor of not dying of cardiovascular disease: NEJM 346:
793, 2002.
And the famous step-two diet for improving LDL and HDL status actually fails
in men and post-menopausal women if they refuse also to exercise:
NEJM 339: 12, 1998.
Despite some pop claims, the "big four" (cholesterol, smoking, hypertension, diabetes)
still account for the vast majority of heart attacks: JAMA 290: 898, 2003.
6. A variety of biochemical lesions (hereditary, acquired) that promote thrombosis
NEJM 338: 79, 1998,
Circulation 86(S III): III-95, 1992, lots more).
Not yet "official", it is probably at least as important a risk factor as diabetes.
7. Other heredity: Important. Currently being sorted out as a risk factor.
You already are familiar with familial hypercholesterolemia, in which there is a defective apoprotein
B-100 receptor (there are many different molecular variants), IDL's are not properly cleared by the
liver and become excess LDL instead, and the "good" receptor-mediated pathway of LDL uptake by
other cells is unavailable.
There are also birth defects involving other apolipoproteins, and those in which there is excess
Lipoprotein A (see below).
Polymorphisms involving apolipoprotein B itself are clearly important in determining coronary risk.
Outstanding as a cause of high LDL is "familial defective apo-B-100", an autosomal dominant
(NEJM 338: 1577, 1998; this alone may kill around 1 person in 1000).
* Some folks, however, have trouble making apo-B at all, which is good if you want to eat lots of
greaseburgers and never raise your LDL: Proc. Nat. Acad. Sci. 92: 1772, 1995.
* Protease inhibitors for HIV infection cause hyperlipidemia and lipodystrophy
by interfering with the breakdown of apolipoprotein B: Nat. Med. 7:
1327, 2001.
* The lipoprotein A allele LpS2 was once reported to be
a potent risk factor for coronary artery atherosclerosis
(Lancet 343: 1194, 1994); this evidently was never confirmed.
HDL is composed of A1 and A2 apolipoproteins.
Apo-A1 seems to have the most to do with removal of cholesterol from membranes.
This is by now quite well-established (Am. J. Card. 91 12E, 2003.
There's even been talk of using A1 instead of HDL as your measure of "good"
cholesterol (Arch. Path. Lab. Med. 121: 678, 1997), but so far it remains
a research topic (Circulation 97: 1784, 1998) Thie may change.
It's been known for over a decade that transgenic mice with lots of A1 get much
less atherosclerosis; those with
lots of A2 paradoxically get more. Science 261: 469, 1993.
A mutated apoA-1 that causes severe atherosclerosis in humans: J. Am. College Card. 44: 1429 2004.
Familial combined hyperlipidemia, i.e., high VLDL's, high LDL's, low HDL's ("my triglycerides and LDL
both run high"), affects about 1% of folks and is a
major coronary risk (3-10x increase over baseline).
Patients are now considered a subgroup of the "syndrome X" family
since most show central adiposity.
The biochemical lesion is overproduction of apo B in the lipoproteins
(review J. Clin. Endo. Metab. 89: 2601, 2004).
The illness is obviously polygenic. It is expressed only in adults.
A mouse model has mutations at both apoprotein C-III and the LDL receptor (Science 275:
391, 1997). One human gene is apolipoprotein A-II
(Nat. Gen. 18:
369, 1998.
Tangier disease is an autosomal recessive disease
in which patients have near-zero HDL levels, low LDL levels,
and extensive deposition of cholesterol esters in the tissues.
Patients have orange
tonsils, a neuropathy, and precocious atherosclerosis. Even heterozygotes
have many foam cells, low HDL's, and increased coronary risk.
Gene (ABCA1) and syndrome:
Nat. Genet. 22: 352, 1999; the missing protein is responsible
for taking cholesterol to the surface of cells to be carried off
by apo-A-I. There is also a dominant low-LDL syndrome
at this locus
("familial hypoalphalipoproteinemia, also an atherosclerosis risk:
Lancet 354 134, 1999).
Despite older ideas, people with hereditary lipoprotein lipase deficiency ("type I hyperlipidemia")
are indeed
prone to accelerated
atherosclerosis (NEJM: 335 848, 1996).
* TLR4 is a newly-discovered molecule that has to do with how brisk one's
inflammatory responses are. People with alleles that produce a subdued
response to bacterial invasion are more susceptible to serious infection,
but protected from atherosclerosis (NEJM 347: 185, 2002).
And yet other folks run high Lp(a)
("lipoprotein Lp(a)", LDL with an apoprotein A attached), which puts them at risk.
Excess Lp(a) runs in families and is constant through life.
It can and often does kill somebody with no other coronary
risk factors (Arch. Int. Med. 157: 1170, 1997). Known mechanisms
include:
- LDL oxidizes too easily;
- extra cholesterol gets deposited
- impaired fibrinolysis (it probably blocks plasmin binding sites)
* Lp(a) is lowered by niacin, male and female hormones, and alcohol
drinking, but not by other means (Am. J. Med. 110: 22, 2001).
Lp(a) review NEJM 349: 2108, 2003.
* Polymorphisms for Apolipoprotein E
received considerable attention during the 1990's,
but there were apparently no reproducable findings.
* Platelet glycoprotein IIIa variant, rendering platelets stickier and therefore placing a person at risk
for coronary disease??? Yes: NEJM 334: 1090, 1996; Blood 94: 46, 1999;
Circulation 104: 140, 2001. No: Lancet 349: 385, 1997'
Lancet 353: 708, 1999; Circulation 102: 1901, 2000. Also watch the "human platelet antigens".
The good news is that these genetic factors (as well as the havoc of hypertension) can be
more or less neutralized by lowering LDL levels, by whatever means (Science 272: 629, 1996; Br.
Med. J. 313: 1273, 1996).
* Common longevity mutation in cholesterol-ester transfer protein, which
produces abnormally large LDL's and HDL's: JAMA 290: 2030, 2003.
8. Low HDL & elevated fasting triglycerides.
Perhaps the HDL assay is most useful as a marker for the as-yet-poorly-understood
metabolic syndrome X or insulin resistance syndrome, with hypertension, insulin resistance, low HDL,
high fasting triglycerides, truncal and a serious coronary risk even
with normal LDL / total cholesterol.
This is a hot topic right now. Of course, the mainstay of therapy
is diet and exercise (weight loss is key: Am. J. Card. 87: 827, 2001).
Reviews Am. J. Epidem. 152: 897, 2000,
Am. J. Card. 84(1A): 11J, 1999;
Circulation 100: 123, 1999.
* Some fat in the liver, and elevated liver enzymes, is also typical:
QJM 92: 73, 1999.
* Watch for
- resistin, produced by the adipocytes, as etiologic
- inclusion of Stein-Leventhal, hirsutism-obesity in older women,
non-alcoholic steatohepatitis, and endometrial cancer in the constellation
- more on the rat model, induced by feeding a greasy American-type diet (Hypertension 37: 1323, 2001)
- treating it with diet and exercise
- new categories of medications to treat the defect at the cellular level (* including
the altered nuclear membrane receptors: NEJM 353: 604, 2005)
9. Elevated levels of homocysteine.
Homocysteine can be elevated because of (1) an inborn error of metabolism, or (2) low intake of folic
acid, or (3) low intake of vitamin B12. People with the inborn errors get horrendous atherosclerosis early in life.
* Even a common, mild mutation in methylenetetrahydrofolate reductase
is a serious risk factor for atherosclerosis: Circulation 99: 2361, 1999.
Most vegetarians have mildly elevated
serum homocysteine levels because of a relative B12 deficiency (Clin. Chim. Acta 326:
47, 2002; Am. J. Clin. Nutr. 78: 131, 2003;
Ann. Nutr. Metab. 46: 73, 2002). Of course vegetarians
overall have less, rather than more, atherosclerotic morbidity and mortality,
though this is not under intensive study recently;
pure vegetarians with good genes
usually have total cholesterol less than 150 unless
they eat a lot of saturated vegetable oil (Am. J. Card. 83: 816, 1999).
Stay tuned.
Homocysteine, in turn...
- is a mitogen for vascular smooth muscle;
- damages endothelium (possible mechanism Circulation 105: 1037, 2002);
- makes blood hypercoagulable.
There's now pretty good evidence that elevated blood homocysteine (as in folks who are deficient in
folic acid, which is still probably true for many Americans) is a major independent risk factor for atherosclerosis
(NEJM 332: 234, 1995; JAMA 281: 1817, 1999;
lancet 355: 523, 2000;).
and
a
prospective series (JAMA 275: 1929, 1996). Review for everybody: Am.
Fam. Phys. 56: 1607, 1997.
Among the homocysteine-challenged.... Making early atherosclerosis shrivel with B6 and folic acid
works: Lancet 355: 511, 2000. Soon everybody may be taking betaine supplements.
NOTE: Despite all of the above, women are relatively protected from atherosclerosis until
menopause. Afterwards, their risk increases rapidly to equal men's. Post-menopausal estrogen is
protective (other bad press notwithstanding:
Ann. Int. Med. 135: 939, 2001), and the addition of progesterone does not remove this protection: NEJM 335: 453, 1996.
* The mechanism by which estrogens protect remains obscure.
One idea is that estradiol greatly up-regulates FasL expression on endothelium,
which keeps out the inflammatory cells: Circulation 104: 2576, 2001.
NOTE: People of Japanese ancestry, living in Japan,
have traditionally relatively low risk for atherosclerosis. This has changed
dramatically over the past two decades (Arch. Int. Med. 160: 2297, 2000).
When they move to America and become Americanized, their risk approaches that of the rest of us.
NOTE: Finland and Scotland have slightly higher rates of atherosclerosis (reflected in rates of death
from ischemic heart disease). The United States probably ranks next, followed by the rest of the
"Western World", and far more than Japan or the poor nations.
When a third-world country develops rapidly, so does atherosclerosis (Atherosclerosis 153:
9, 2000).
NOTE: The French, with a very high-saturated-fat diet (that's part of why French cooking is so
good), have a relatively low rate of atherosclerosis. This is probably due to their tremendous alcohol
consumption; there was talk in the 1990's about
tannins in red wine inhibiting oxidation of LDL's
in the French, but nothing much lately.
NOTE: * Watch the impact of carotenoids and their close kin
in preventing atherosclerosis. Works for mice.... Circulation 103: 2922, 2001.
NOTE: The Inuit ("Eskimos"), who eat a lot of fat, are supposedly protected by omega-three fatty
acids.
You already know that a diet high in saturated fat (mostly of animal origin)
or trans-unsaturated fat ("hardened" fat,
think of margarine) raises LDL cholesterol.
NOTE: "No-cholesterol" dietary items are still LDL-raisers and supposedly
atherogenic if rich in saturated fat.
NOTE: After 1991, the coronary artery mortality in Poland plummeted.
Probably it's from a better diet, with more fresh fruits and vegetables
and vegetable fats
and less lard (BMJ 316: 1047, 1998).
NOTE: You can go nuts trying to keep track of which factors and their remediation affect, correlate
with, and "are associated with" which other factors, listed or rumored to be important in
atherogenesis. I seriously doubt that "stress", independent of these other variables, is a significant
risk factor for atherosclerosis. However, higher serum epinephrine levels probably would increase a
person's risk of sudden cardiac death in a potentially rhythm-disturbing situation, all other things
being equal.
NOTE: I am still not aware of any reason to
believe that obesity is a risk factor for atherosclerosis except insofar as it is related
to the above (i.e., high cholesterol from bad diet, smoking, hypertension, diabetes, lack of exercise, metabolic syndrome X).
Obesity (especially "central obesity",
i.e., the dude's butt-crack shows over his beltline when he squats) produces
the hormone resistin, which renders muscle and liver resistant to the effects of insulin
and maybe does other things.
I am also not impressed with isolated
fasting triglyceride levels as an independent risk factor (neither is the
NIH consensus panel JAMA 269: 505, 1993). Iron overload may also
be a risk factor maybe by oxidizing LDL
(yes! Circulation 96: 3300, 1997;
no! NEJM 330: 1119, 1994), right now the no's seem to have won.
Claims about coffee has repeatedly flopped.
The "baldness is an independent risk factor" article (JAMA 269:
998, 1993; even a bright kid could point out methodologic howlers) was sponsored
by the hair-restorer folks anticipating some
lawyer finding "a higher rate of MI's in people using hair-restorer".
NOTE: Consensus panel on lipid profiling (JAMA 269: 505, 1993) recommends screening
HDL-C along with routine cholesterol screens, but can't find much reason to check triglycerides or
consider them an independent risk factor.
"Atherosclerosis as an infectious disease."
You will be told that that micro-organisms
cause atherosclerosis, both by acting at the sites of the lesion or
and by "increasing the total body burden of inflammation."
Your lecturer does not believe this is true. You can decide for yourself, of
course, but here are the facts.
From time to time, people find what seem to be bits of microbes in atherosclerotic plaques and suggest the bugs are
etiologic. DNA sequences from various bugs get reported fairly often
in plaque debris. Immunofluorescence identifies antigens from these
bugs in the debris as well. Since many different "microbes"
have been identified in this way (including the very unlikely Helicobacter
pylori), and since the bacteria themselves are never convincingly
visualized, the obvious explanation is that the plaque grunge itself
soaks up whatever microbial debris may be in the bloodstream.
The CMV-causes-atherosclerosis flap of the 1980's came to nothing.
Now it's
chlamydia-in-your-plaques (J. Inf. Dis. 175: 883, 1997;
negative study Br. Med. J. 318: 1035, 1999, J. Am. Coll. Card. 41: 1482, 2003;
two more Br. Med. J. 321: 204 & 208, 2000).
Even the proponents admit the case is hardly made: JAMA 288: 2724, 2002. The inflammation
in plaques hardly resembles what you see in
trachoma, psittacosis, lymphogranuloma
venereum or other known chlamydial illnesses -- these display spectacular proliferation
of lymphoid germinal centers and abundant plasma cells, and/or suppurating
granulomas.
Chlamydia are easy to see in the illnesses they obviously cause,
but in atherosclerosis the actual organisms (rather than just their DNA
or antigens) remain incredibly elusive.
The most recent sighting is Acta. Biol. Hung. 86:
233, 2005 and the "chlamydia" were calcified...
Draw your own conclusions.
Correlating the presence of a microbe and severity of atherosclerosis
makes for an extremely easy "scientific study."
And these studies are driven by the hope that atherosclerosis might respond
to an antibiotic-based regimen as has worked so well for stomach ulcers.
A key difference is that anybody can see the bacteria in stomach ulcers, and
nobody can actually see them in athersclerosis.
And a conspicuous lack of controls distinguishes
most of the "positive" studies I've seen.
For example, a handful of studies finding that people with helicobacter in their stomachs
get worse cornary atherosclerosis fail to control for tobacco smoking
and dietary habits. (We'll let you find this stuff on your own.)
Most recently the talk is about "infectious burden", i.e., the more different usual suspects that you're
making antibodies against, the greater your risk of dying of a heart attack
(Circulation 105: 15, 2002). The fact that the "usual suspects" now
include genital herpes and stomach helicobacter invites the idea that
old folks who are sicker are more likely to have polyclonal B-cell activation, which is simply
common sense.
C-reactive protein is presently the subject of much
excitement, since serum levels in the absence of the acute phase reaction
seem to correlate with the extent of atherosclerosis in both humans and
animal models of atherosclerosis.
In animals, C-reactive protein is found in the plaques between the cells in all stages
of their development (co-localizing with apolipoprotein B), and seems to be soaked up from the plasma
(Am. J. Path. 167: 923, 2005).
There's much talk about the "proinflammatory phenotype" (J. Clin. Endo. Metab. 90:
4549, 2005), i.e., the person who's likely to have high C-reactive protein levels in the
absence of obvious inflammation. Surprise! These people are older and have much
fatter, have higher triglyceride levels, higher insulin levels (i.e., insulin resistance), and
higher leptin levels -- all obviously involved with atherosclerosis. For some reason,
other acute-phase-reaction markers (fibrinogen, stimulated interleukin beta,
some more obscure proteins)
also average higher.
All this says to me is that there is some link between the C-reactive protein
system and lipid metabolism. The conclusion that people with atherosclerosis
harbor more smoldering infections hardly seems warranted.
Supporting your lecturer's skepticism is a single study that addressed the
obvious question. Mice with a genetic predisposition to atherosclerosis
get exactly the same lesions whether they are germ-and-virus free or have
the usual microflora (J. Exp. Med. 191: 1437, 2000.) No one has
repeated this work, and this fact alone tells me something about the whole
field.
NOTE: There are several situations in which development of atherosclerosis is accelerated. These
include
- previous radiation to an artery;
- arteries in transplanted hearts (inflammation, of course:
Circulation 106: 1536, 2002)
- vein grafts in
coronary bypass surgery
- coronary arteries after angioplasty
- situations in which the walls of
arteries are burdened with immune complexes.
In these situations, "endothelial damage" and
"thrombosis" appear to be critical. Read all about it: Mayo Clin. Proc. 66: 818, 1991.
Okay, atherosclerosis is actually a pattern of injury.
{03473} atherosclerosis, in a vein graft
{06581} atherosclerosis after radiation
The innocent precursors: (anatomy: Am. J. Path. 143: 1444, 1993)
{11057} fatty streak
{25024} fatty streak
{41533} foam cells
Don't worry about fatty dots, lone macrophages with cholesterol.
Every toddler in the world probably has fatty streaks, masses of lipid-rich foam cells (mostly
macrophages as this stage) in the intima. These impart a pretty two-tone appearance to the intima of
most everyone's aorta, without causing other problems. Most researchers now consider these
precursor lesions to common-type serious atherosclerosis.
Not yet explained: (1) Their distribution differs from serious plaques; (2) Their presence seems
unrelated to diet, etc., (3) They seem to regress later in life as fibrous plaques grow more severe.
We've got plenty still to learn about the pathogenesis of the fatty streak, but parts of the picture have
recently become clear.
Fatty streaks result from macrophages taking up LDL cholesterol, but the LDL must first be altered
to "oxidized LDL" ("Ox-LDL", i.e., with its cholesterol and/or unsaturated fat peroxidated) taken up
by an exotic "Ox-LDL receptor" (cloned Nature 385: 73, 1997) on the macrophage surface, and
processed via the "scavenger pathway". The alteration can be brought about by endothelium or
smooth muscle.
The risk factors have little to do with fatty streaking, which is universal. Boys have more than girls,
blacks more than whites, it takes over maybe 30% of the surface by the teens.
The time bombs: Fibrous plaques
{11054} fibrous plaques
Later in life (and it all depends on risk factors), a person develops fibrous plaques. These are masses
of cholesterol-rich cells
with an overlying fibrous cap. There may be dystrophic calcification,
extensive fibrosis and/or smooth muscle hyperplasia in the plaque, and some calcification.
Cholesterol-laden cells appear as foam cells; these are usually both of smooth
muscle and macrophage origin. When they die, there will be cholesterol needles
(remember these?) and grumous debris. ("Grumous" is a charming near-synonym for "grunge", i.e.,
granular, semi-solid material.)
Despite all the current excitement about "inflammation as the cause of atherosclerosis",
the inflammatory cells (T-lymphocytes)
are usually found only as little clusters at the edges of the plaque.
Marvels of technology: Today's intraluminal ultrasounds and MRI's have reminded
clinicians of the existence of soft, mushy cores of plaques. These are now
called vulnerable plaque or high risk plaque, i.e., where you're likely
to have a rupture
or bleed, as opposed to fibrous stuff which isn't
going to rupture or bleed. MRI's: Am. J. Card. 88(2A): 42E, 2001.
In acute coronary occlusion, angioplasty fails to establish re-flow
in up to 30% of cases. We now know that many of these people actually
have the grunge ("plaque gruel") released from the plaques by the
procedure, and this itself plugs the artery (Circulation 106: 1672, 2002).
* Watch "pregnancy-associated protein A", present in vulnerable
plaque, as a serum marker for having just ruptured one.
I predict this will prove to be of limited specificity for
coronary disease, since people with
generalized atherosclerosis often have a bare plaque somewhere
other than the coronaries. But see NEJM 345: 1057, 2001.
While we are talking about calcium...
"Chelation therapy" is an old "alternative treatment" for atherosclerosis.
The patient is given a calcium chelator, usually EDTA, by vein, and told that
this removes the plaques, which are made from calcium. This causes tingling
of the fingers (transient hypocalcemia) which the practitioner tell the patient is due
to improved circulation to the fingers. No need to belabor why this is nonsense,
and of course the empirical work has shown no effect on plaques. "Chelation therapists"
promote healthy lifestyles and perhaps they serve a useful function for this reason.
I believe that anyone practicing "chelation therapy" nowadays is knowingly deceiving the public.
 Coronary graft vascular disease
Coronary graft vascular disease
Pittsburgh Pathology Cases
In at least many cases, atherosclerotic lesions are monoclonal, suggesting that
Nowell's law / natural
selection operates in their pathogenesis. This isn't surprising, especially since (1) we now know that
oxidized-LDL is mitogenic for macrophages, and (2) the smooth muscle of
the aorta itself is made of large groups of clonal cells
(Am. J. Path. 152: 913, 1998). However, the old claim that each plaque arises from a
single cell has now been amply refuted.
Much work now indicates that progression from the fatty streak to the fibrous plaque is at least in
part the result of incorporation and organization of thrombi (* "the Rokitansky theory"). Most
fibrous plaques are rich in material that immunostains as fibrin (though this is absent from normal
artery or fatty streaks).
The distribution of the fibrous plaques is fairly predictable. Probably
because of increasing turbulence (farther downstream, and running up
against the iliac bifurcation), they increase
centrifugally in the aorta. They are especially common at bifurcations "where turbulence damages
the endothelium". Unfortunately, the carotid bifurcation and origin of the left anterior descending
coronary artery are favorite sites. Renal artery ostia are vulnerable, though the rest of the renal
artery is spared. Iliac arteries get it much worse than brachial arteries. The low-pressure pulmonary
arteries are almost never seriously affected; finding any plaques at all strongly suggests pulmonary
hypertension. p>
The killers: Complicated plaques
{11060} the nasty stuff
{14216} the nasty stuff
{25461} the nasty stuff
{53265} the nasty stuff
 Atherosclerosis
Atherosclerosis
Prosthesis in place
Urbana Atlas of Pathology
As a person continues to be at risk for atherosclerosis, the plaques become complicated. Any of the
following unpleasant things can happen:
- The surface of the plaque becomes damaged, resulting in thrombus formation.
Platelets, fibrin, or both accumulate wherever the endothelial cells are damaged or lost. Platelets
produce such factors as platelet-derived growth factor, transforming growth-factor beta, and others.
Fibrin makes endothelial cells migrate (rendering the surface permeable), causes vascular smooth
muscle to proliferate, presents a surface on which LDL may accumulate, binds the LDL variant
Lp(a) (i.e., LDL with a bound apoprotein A molecule) that accumulates in the plaque with the
fibrin, etc., etc. Fibrin degradation products also enhance vascular permeability.
The thrombus can embolize if the artery is large, or plug the lumen if the artery is small (i.e., a
coronary or cerebral artery). This is probably the cause of a majority of myocardial infarcts and
cases of unstable angina pectoris.
If the "Rokitansky theory" is correct, the thrombus is even more likely to become incorporated into
the plaque, making it grow. For an update on thrombus formation on top of plaques, see Ann. Int. Med. 134:
224, 2001.
Endothelial damage alone might result from "high LDL" (see above), a virus (yeah, sure), or shear
forces of flowing blood (plausible, since atherosclerosis is worse at bifurcations). As noted, the body
responds by accumulating lipids and monocytes with cell-derived growth factors causing smooth
muscle cells to proliferate. This probably begins the spontaneous atherosclerosis process.
Cracking-fissuring of the fibrous cap (review: Circulation 82(S II): II-47, 1990) leads to deposition
of at least a platelet layer, and often a real thrombus. There are often cracks in coronary arteries and
little thrombi even in patients dying of something other than MI.
If the injury reaches the media, the clotting cascade will surely be activated, smooth muscle cells
will migrate in, and fibrosis will occur. And thrombin appears to be mitogenic for smooth muscles cells
(either directly or indirectly).
Since atherosclerosis is a patchy process, it would seem reasonable to think that plaques exacerbate
local conditions that contribute to their own growth. Two such mechanisms could be thrombosis
and turbulent blood flow.
- The fibrous cap cracks, discharging grumous debris into the lumen. This can result
in embolization if the artery is large (heart attack, renal shutdown, King Herod's disease), or
thrombosis.
- One of the weak little arteries that develops in the plaque ("neovascularization")
bursts, ballooning the roof of the plaque against the opposite wall of a small artery.
{06524} lethal hemorrhage into a plaque in a coronary artery
 Hemorrhage into a plaque
Hemorrhage into a plaque
Caused death
ERF/KCUMB
- The plaque deprives the inner media of its nutrients, causing it to weaken and
balloon out ("aneurysm").
This is most common in the big arteries (why?)
(* Future pathologists: Sometimes a plaque itself may thin the wall of the
aorta so much that it bursts outward, with fatal results:
AJFMP 17: 38, 1996).
The good news: It's reversible
Although the idea is little-known, there is abundant evidence from animal work (and some from
humans) that atherosclerotic lesions can and do regress, if the risk factors are corrected.
How the cholesterol leaves the plaques when the LDL situation
improves: Circulation 99: 1959, 1999.
In the regressed lesion, the intracellular lipid vanishes, the extracellular lipid where the cells have
died diminishes, the fibrous cap remodels and flattens, and the endothelial damage overlying the
fibrous cap heals. See Am. J. Card. 65: 33F, March. 20, 1990.
For an update on plaque regression using statins, see J. Am. Coll. Card. 46: 106, 2005. This is now mainstream;
I predicted this in 1994.
* The "Pathobiological Determinants of Atherosclerosis in Youth Study"
(JAMA 281: 727, 1999) looked at people aged 15-34 and under who
died of unrelated causes, and found fatty streaks to ubiquitous and
fibrous plaques fairly often. Any pathologist could have showed you without
your having to spend any money, Uncle Sam. Accepting the study's conclusion
that "primary prevention of atherosclerosis must begin in childhood
or adolescence" requires us to make the dubious assumption that
today's harmless streak or bump
must be tomorrow's killer plaque, and that today's clean
coronary is far more likely to be clean in 30 years. Given the
suddenness with which severe atherosclerotic lesions appear (consider
the effect of female menopause) and regress (see below), that's
asking us to assume a lot.
THINK! In the space below, review how each risk factor or intervention might work at the
molecular and chemical levels:
High LDL is bad
Cigaret smoking is bad
High blood pressure is bad
Diabetes is bad
An aspirin a day is good (HINT: Thrombi and platelets,
maybe "reduced inflammation".
* The British anti-platelet study: Br.
Med. J. 308: 81 & 159, 1994; aspirin sounds good for those at high risk for myocardial infarction,
but for those at low risk, the hazard of hemorrhagic stroke may outweigh the benefits). Aspirin
review: Am. Heart J. 137: S-9, 1999.
NOTE: Don't confuse atherosclerosis with the notable non-disease, Monckeberg's medial calcific
sclerosis (see below).
NOTE: Together, atherosclerosis, Monckeberg's, and the two kinds of arteriolar sclerosis listed
below are arteriosclerosis. In other words, avoid using that word altogether.
* NOTE: When diet and exercise fail....
Cholestyramine / colestipol: Binds cholesterol in the gut
Niacin: Decreased LDL and VLDL synthesis
Gemfibrozil: Enhances VLDL clearance
Statin family: Blocks cholesterol synthesis
MONCKEBERG'S MEDIAL CALCIFIC SCLEROSIS
Dystrophic calcification (sometimes even ossification) of the media of arteries, typically in older
adults.
This is a common, banal, pretty much harmless process. At worst, it can widen one's pulse pressure,
or make "radial artery blood-gas sticks" difficult and hazardous.
On the "plus" side, it makes for some great x-rays.
* Evidently the smooth muscle cells produce at least four proteins that indicate
they want to make bone. You can read about it in Circ. 100: 2168, 1999.
ARTERIOLAR SCLEROSIS ("arteriolosclerosis")
Three processes that narrow the lumens of the small arteries and arterioles in some or all of the
body
Intimal fibrosis or (better) "fibroelastic hyperplasia",
is the slow buildup of fibrous tissue (usually with some layers of elastic)
in the intima of a small artery. It's a part of aging, and is exacerbated
by high blood pressure. It involves smaller arteries (rather than
the larger ones, as in
atherosclerosis) and doesn't feature the lipid buildup. It also spares
the arterioles.
Hyaline arteriolar sclerosis: slow buildup of basement-membrane type material, eventually
obliterating the cellular structure of the wall and narrowing the lumen.
Mostly the arterioles are involved.
Extremely common. The causes are
- prolonged high blood pressure from any cause;
- prolonged hyperglycemia from any cause.
- radiation injury (typically iatrogenic, an expected result of radiation therapy)
- * focal-segmental glomerulosclerosis / hyperfiltration lesion in the failing kidney (more about this soon)
No one really knows why any of these causes "hyaline arteriolosclerosis", but the
anatomic pathology is impressive.
Hypertension is the least potent. The effects on tissue perfusion, and probably on the sympathetic
regulation of blood pressure, are not salutary.
Future pathologists: Look in the fat just outside the adrenal capsules to get a good idea about the
extent of systemic hyaline arteriolosclerosis. Lots of hyaline change of the small arteries here is a
great marker for "triple-P" (pretty poor protoplasm). "Binswanger's encephalopathy" is a dread,
Alzheimer-like dementia caused by hyaline arteriolosclerosis of the brain.
If you like, you can consider amyloidosis of small arteries, which hyalinizes
but is less likely to cause much stenosis,
to be a form of it. No one will argue or care.
{11777} hyaline arteriolar sclerosis
{40267} hyaline arteriolar sclerosis
{40347} hyaline arteriolar sclerosis
 Hyaline arteriolar sclerosis
Hyaline arteriolar sclerosis
Photo and mini-review
Brown U.
Hyperplastic arteriolar sclerosis: Concentric, often rapid proliferation of the intimal (or sometimes smooth muscle) cells
of an arteriole.
"Onion-skin
arteriole".
Fortunately uncommon. The causes are
- malignant hypertension (i.e., very bad high blood pressure that damages the vessels)
- bad pulmonary hypertension
- scleroderma (fingers, kidneys, other)
- hemolytic-uremic syndrome (E. coli burger disease, kidneys especially)
- * Degos's disease (a curious skin disease)
* What's probably happening is failure of endothelial cells to undergo
apoptosis when they should: Nat. Med. 4: 222, 1998. Look for
novel treatments based on this!
Don't confuse this with the fibroelastic hyperplasia of the intima of
the small arteries in common high blood pressure and old age.
{39559} hyperplastic arteriolar sclerosis in pulmonary hypertension
{24854} hyperplastic arteriolar sclerosis, scleroderma kidney
 Hyperplastic arteriolar sclerosis
Hyperplastic arteriolar sclerosis
WebPath Photo
Note that all these are processes that specifically damage the intima of vessels, which
presumably
undergo hyperplasia in response. This is a much more aggressive process. (You could think of it as
a callus of the endothelium.)
Note that any of these processes can be severe enough to cause some necrosis of the vessel.
Malignant hypertension is usually this severe.
Don't confuse either of these processes with the inexorable fibrous thickening of the intima of small
arteries in mild hypertension and normal aging. This is so common and so important that it doesn't
have a name beyond "intimal fibrosis".
Transplant vasculopathy is a concentric fibrous thickening, mostly confined to the intima, in
allografts (heart, kidney, liver, others) that have survived for a long time; the process develops rather abruptly, and while
immunity must be a factor, it cannot be the only explanation. See Am. Heart. J. 129: 791, 1995.
 Transplant vasculopathy
Transplant vasculopathy
WebPath Photo
THE VASCULITIS FAMILY
Polyarteritis nodosa
Due to hepatitis B infection (antigen-antibody complexes), anti-myeloperoxidase disease ("anti-neutrophil cytoplasmic
antibody disease"), or "idiopathic".
We've already studied this dread, protean disease. Remember it's an important cause of infarcts
anywhere in the body except lung.
Leukocytoclastic vasculitis
Generally type III immune injury of the venules, often diagnosed on skin biopsy (the patient has
"palpable purpura"). Common, but infarcts and serious damage are fortunately rare.
"Leukocytoclastic" refers to the dead neutrophils lying about, visible as nuclear dust.
{14284} leukocytoclastic vasculitis
{14286} leukocytoclastic vasculitis
{14287} leukocytoclastic vasculitis
{14289} leukocytoclastic vasculitis
{14290} leukocytoclastic vasculitis
{14292} leukocytoclastic vasculitis
{14293} leukocytoclastic vasculitis
{14294} leukocytoclastic vasculitis
{14295} leukocytoclastic vasculitis
{14296} leukocytoclastic vasculitis
{14298} leukocytoclastic vasculitis
Mostly this results from taking medicines. Less common causes are cryoglobulinemia (how?), lupus
and its kindred, and the antigenemia of HBV and malignancy.
Wegener's granulomatosis
You know anti-proteinase 3 disease. Lung cavities, segmental necrotizing glomerulonephritis with crescents,
and vanishing nose, all with granulomas.
Churg-Strauss disease
This is an eosinophilic vasculitis accompanied by asthma, usually of new onset.
We've already covered this disease, which is a great mimic (Chest 128:
1047, 2005). The response to glucocorticoids is usually better than
in other vasculitis syndromes.
{38497} old burned-out Wegener's, without good granulomas
Temporal arteritis ("cranial giant cell arteritis")
A disease of older (>60) adults (> 2:1), still of unknown etiology, in which the macrophages seem to
become
angry with the internal elastic membrane of the arteries of the external carotid system.
"Jaw claudication" (tired jaw on chewing) is a picturesque syndrome, but sudden blindness (the
dread complication) is a catastrophe.
Many of these patients also suffer from pain and weakness in the muscles, the distinctive
polymyalgia rheumatica. Future clinicians: The diagnosis is supported by finding everything
normal on physical exam except perhaps for tender temporal arteries, plus normal labs except for a
high "sed rate".
Only recently has it become clear that there is systemic overproduction of
interleukins 1 and 6 for some reason, and activation of macrophages in the vascular intima.
There is still a great deal that' s unknown (Ann. Int. Med. 139: 505, 2003).
Prove your diagnosis with a temporal artery biopsy, which may or may not show granulomas on the
inner elastic membrane. There is also a striking non-granulomatous fibrous
proliferation of the intima.
When in doubt, treat with prednisone.
How long to treat: Arch. Int. Med. 159: 577, 1999.
Polymyalgia rheumatica can occur in young people and/or in
the absence of elevated sed rate (Arch. Int. Med. 157S:
317, 1997). When in doubt, treat.
* Future pathologists: Biopsies remain positive even after several weeks of glucocorticoid
therapy (Br. J. Ophth. 86: 530, 2002).
{22095} temporal arteritis
{22096} temporal arteritis
{22098} temporal arteritis
{24777} temporal arteritis
{28019} temporal arteritis
Takayasu's pulseless disease ("aortic arch disease", etc.)
A fortunately-rare, idiopathic disease of younger adults (almost always) in which the aortic arch and
its great branches thicken and their ostia become stenotic, strangling off blood flow to the upper part
of the body.
No one knows the cause, and the histology is nonspecific, with granulomas, lymphocytes, plasma
cells, and so forth, in addition to the fibrosis and contraction.
* The molecular biology of temporal arteritis and Takayasu's
is evidently similar. What's known: NEJM 349: 160, 2003. Watch
for aspirin to be added to the glucocorticoid regimens, to prevent
platelet-related intimal fibrosis in both diseases.
{48983} Takayasu's
* Cogan's disease is another thankfully-rare
disease usually affecting young adults. It features abrupt onset of nerve deafness,
interstitial keratitis, and/or a systemic vasculitis often with aortic aneurysm
formation. It's apparently caused by an autoantibody against inner ear and endothelium
(Lancet 360: 915, 2002).
Kawasaki's disease ("mucocutaneous lymph node syndrome";
Ped. Clin. N.A. 46: 313, 1999; Am. Fam. Phys. 59:
3093, 1999; Lancet 364: 533, 2004)
A febrile disease that resembles adult polyarteritis nodosa histologically but occurs in babies and
toddlers, mostly of Japanese ancestry (no matter what country).
The fact that almost all patients are around 2-5 years, the fact that occasionally
an older child or adult gets the disease, the fact that there are outbreaks,
and the fact that babies don't get it
as long as they have maternal antibody all tell me the cause is an unidentified, ubiquitous virus.
You'll want to see five of these six signs:
- fever (will last more than five days)
- non-purulent conjunctivitis in both eyes
- rash
- red cracked lips and/or
strawberry tongue and/or red oral mucosa
- red palms and soles; later they desquamate
- a big (1.5 cm or more) node in the neck
Most patients are of Japanese of Korean ancestry, regardless of where they live,
but no HLA links are found.
The most serious concern is coronary vasculitis, which causes myocardial infarcts. Healing can
produce coronary aneurysms, etc. See Arch. Dis. Child. 87: 145, 2002.
There are a host of immune abnormalities,
and presently folks are talking mostly about
sensitization to a bacterial superantigen (i.e., something
that makes large numbers of lymphocytes go crazy).
Toxic shock syndrome, caused by a superantigen, is a similar
illness. Yet the substance causing Kawasaki's remains unidentified.
See J. Clin. Imm. 15(6S): 11-S, 1995; Ped. Inf. Dis. 19: 91, 2000.
* By electron microscopy, the endothelial cells are separated and perforated,
rendering them hyperpermeable; the molecular explanation remains elusive
(Circulation 105: 766, 2002).
We treat Kawasaki's with aspirin and intravenous immunoglobulin. The
outcome is good unless coronary disease becomes apparent.
 Buerger's disease ("thromboangiitis obliterans": review
Angiology 47: 419, 1996)
Buerger's disease ("thromboangiitis obliterans": review
Angiology 47: 419, 1996)
A disease of
smokers, usually young men,
in which the small neurovascular bundles in the extremities
become inflamed and undergo thrombosis.
No one has a clue as to the real etiology, beyond the link to cigaret smoking. The typical patient,
after losing all his fingers, holds his cigaret between his last two toes. Not a pretty sight.
The prognosis is hopeless unless the patient stops smoking.
The anatomic pathology remains poorly worked-out. Neutrophils touching
giant cells within thrombi is supposed to be characteristic.
The most recent study
(Virchows Archiv 436: 59, 2000) found instead that an intact
internal elastic membrane, fibrosis much worse in the adventitia than
anywhere else, endothelial swelling in the vasa vasora, and onionskinning
of recanalization vessels were most helpful.
Infectious arteritis
Rickettsial disease, syphilis, septic emboli (look for "Roth's spots!"), walls of abscesses, and a host of
others.
Worth mentioning here: A mycotic aneurysm is a spot at a branch-point of an artery where a septic
embolus (usually) has lodged and set up an infection, weakening the wall. ("Mycotic" is an
unfortunate misnomer, since fungi aren't usually the culprits.)
Raynaud's disease & phenomenon
Spasm and occlusion of the arteries supplying the fingers, which turn white, then red, then blue.
Triggered by cold weather, it's most often idiopathic; known causes range from vasculitis syndromes
to operating jack-hammers.
Scleroderma patients and some others have this process greatly exacerbated by hyperplastic
arteriolar sclerosis in the digital arteries.
If it's a bother, get out the calcium-channel blockers, and/or a nice warm pair of gloves.
{24503} Raynaud's
{25459} Raynaud's
{39657} Raynaud's
{39654} Kawasaki's?
{39655} Kawasaki's?
{48983} Takayasu's
* Erythromelalgia
This thankfully-rare
pain syndrome probably results from
opening of arteriovenous channels and closure of precapillary
sphincters.
Long-mysterious, it's now pretty clear that it's a small-fiber
neuropathy (Arch. Derm. 139: 1337, 2003; Brain 126: 567, 2003).
Lack of nutritive blood flow contributes to the pain,
while the excess non-nutrative blood flow causes a burning
sensation. Victims spend much time with affected areas
socking in ice water.
Erythromelalgia most often involves the feet and maybe hands. There are familial forms,
or the disease can simply appear, usually sometime during adult life.
Hard-to-treat, one group reports success in children using
sodium nitroprusside (Arch. Dis. Child. 87: 229, 2002).
AORTIC ANEURYSMS
Atherosclerosis often causes aneurysms,
usually distally in the aorta, above the level of the iliacs.
Exceed 5 cm or so and it's likely to burst (retroperitoneally, intra-peritoneally, intra-duodenal), with
(usually) lethal consequences. Patients may complain first of back pain, etc. Aneurysms are always
lined by thrombus (why?), which sometimes embolizes. Iliac aneurysms are also common; basilar
artery aneurysms seldom rupture but may compress important things.
Occasionally these get infected; the usual bug is salmonella (Am. J.
For. Med. Path. 23: 382, 2002).
* Albert Einstein's physicians knew he had an aneurysm, but when it burst, they got focused on his
gallbladder instead. He died as a result.
{03665} atherosclerotic aortic aneurysm
{11042} atherosclerotic aortic aneurysm
{11048} atherosclerotic aortic aneurysm, repaired
{11642} atherosclerotic aortic aneurysm
{11645} atherosclerotic aortic aneurysm
{18717} atherosclerotic aortic aneurysm
{20305} atherosclerotic aortic aneurysm
{24780} atherosclerotic aortic aneurysm
{25742} atherosclerotic aortic aneurysm
{04589} atherosclerotic basilar artery aneurysm
{24836} atherosclerotic aneurysm, brain
Syphilis causes ischemic damage (by occluding vasa vasora) to the walls of the arteries, and is
famous for causing proximal aneurysms that rupture impressively. Before rupture occurs, look
for the infamous "tree bark" grooves on the intima, as well as occlusion of the coronary and other
ostia and compromise of the aortic valve ring.
It's hard to follow the argument that a proximal aneurysm is always luetic.
Nowadays, syphilis is very rare, and atherosclerosis is common. I wouldn't assume an
ascending
aortic aneurysm is luetic unless the arch is free of significant atherosclerosis.
* "Tree-barking" is just stretch-marks of the aorta. The only reason this is supposed to be
"more typical of syphilis than atherosclerosis" is that, in atherosclerosis, the intima is already
distorted by the atherosclerotic plaques. I know this, because in my several cases of Marfan-style
dilatation of the aortic root, there's always been tree-barking.
{10224} syphilitic aneurysm
{18716} syphilitic aneurysm
AORTIC DISSECTION
Dissecting hematoma, often miscalled "dissecting aneurysm", is blood
that has entered the wall of
the aorta and is following a weak plane ("cystic medial necrosis of
* Erdheim",
actually there are no cysts and no
necrosis, just diminished elastic and maybe a little extra mucoid goo).
Think of the blood acting as a chisel under the strokes of the heart.
 Dissecting aneurysm
Dissecting aneurysm
Photo and mini-review
Brown U.
 "Cystic medial necrosis"
"Cystic medial necrosis"
WebPath Photo
This catastrophe results in progressive compromise of arteries, backwards rupture damaging the
aortic valve and/or coronary ostia, or further backwards rupture into the pericardial sac or pleural
space.
Patients experience a "ripping", agonizing chest pain as the false lumen expands. Michael
DeBakey's claim to fame is having classified and devised the surgical treatment for these people.
Otherwise, the patient's only hope is to have the blood re-enter the lumen, establishing a "double-barrel aorta", with the false
lumen eventually becoming covered with normal endothelium.
Marfan types are more prone to this lesion, but nobody's immune. An epidemic of dissecting
aneurysms occurred among turkeys who acquired lathyrism after eating beta-NH2-propionitrile in
sweet peas.
* Lathyrism occurs in the poor nations after severe droughts, as a result
of eating drought-tolerant sweet peas. There were outbreaks in Ethiopia
and Bangladesh in the 1990's (Lancet 354: 306, 1999; Lancet 362: 1808, 2003).
Minor variants, with limited extension of a bleed into the aortic wall, also exist. "Spontaneous"
dissection of arteries in the neck can cause stroke in young people (NEJM 330: 393, 1994).
Non-surgical management using a stent-graft: NEJM 340: 1585, 1999 (wow!).
{17467} dissecting aneurysm
{18718} dissecting aneurysm
{20222} dissecting aneurysm
{25747} dissecting aneurysm
A pseudoaneurysm, or pulsating hematoma, is a place where
an artery has bled non-fatally, and where the organizing hematoma communicates
with the lumen. Of course, the wall of the "aneurysm" (and it may look
very much like an aneurysm)
will lack the normal elastic layers of an artery.
Coronary artery dissection is thankfully rare. For some reason,
it most commonly occurs after childbirth.
VEINS
Varicose veins
A self-perpetuating process caused by loss of competency in the leg vein valves and support
structures.
We lose our elastic fibers as a result of aging, or blow out valves (by getting fat, having babies,
straining at stool, standing up doing surgery).
The weight of the column of blood doesn't make life easier for the next valve or the support of the
next few cm of vein. Get elastic leg wraps and hope for the best. If it gets too hard to pump blood
back to the heart by way of the veins, or the weight of the column of blood causes continuous micro-hemorrhages, you will see
the familiar hemosiderin stasis pigmentation and/or ischemic stasis ulcers.
Looks similar: post-thrombophlebitis syndrome, with stasis changes
due to damage to the valves after an episode of deep-vein thrombosis.
Stasis ulcers themselves are a very common, very hard-to-treat problem
of older folks. Older explanations ("the poor circulation produces hypoxia")
are being supplemented by new work (the weight of blood causes capillaries to
rupture, with red cells and plasma proteins being extravasated, with
local cytokine activation; Surg. Clin. N.A. 83: 671, 2003.) This fits with there usually being pigmentation
here, and with the accompanying local fibrosis (lipofibrosclerosis).
 You already know from physiology about esophageal varices and hemorrhoids as evidence of portal
hypertension.
You already know from physiology about esophageal varices and hemorrhoids as evidence of portal
hypertension.
Fortunately, thrombi that may form in varicose veins very seldom embolize.
Thrombophlebitis ("trombone fleabites", better "phlebothrombosis";
reviews Lancet 353: 479 & 1167, 1999)
Thrombosis of a deep vein, most often in the leg. You're already familiar with the causes, and the
dread complication (pulmonary embolus). Usually, pain and swelling result, hence "-itis".
Vicious variants include milk leg ("phlegmasia alba / cerulea dolens", thrombosis of the iliac vein,
around the time of parturition), Budd-Chiari syndrome (thrombosis of the hepatic veins) and dural
sinus thrombosis.
Trousseau's migratory thrombophlebitis affects first one vein, then another. The cause is usually
cancer of the pancreas, less often another adenocarcinoma.
Superior vena cava syndrome
From occlusion, usually from extrinsic compression by lung cancer.
Patients have dusky skin in the head, upper extremities, and upper chest.
"SVC syndrome" can cause a bad
headache just from the markedly increased venous pressure.
Inferior vena cava syndrome
From occlusion, usually by cancer in para-aortic lymph nodes.
Patients have dusky lower bodies and unusual patterns of collateral circulation.
LYMPHATICS
Lymphangitis
Inflammation of lymphatics, usually by a bacterium that's good at invading them (i.e., streptococcus
group A.) You'll see red streaks running along an extremity, etc.
Lymphedema
Compromise of lymphatic draining of the extremities and/or genitalia. The most important causes
are cancer of the cervix, filariasis, iatrogenic (i.e., after the overly-zealous old mastectomies),
autosomal dominant ("Milroy's disease", the lymphatics don't form properly), or "idiopathic" (again,
sometimes the lymphatics don't form properly). Turner's girls often have lymphedema of the hands
and feet.
If there's hyperplasia of the overlying epidermis, it's elephantiasis.
 Lymphedema
Lymphedema
Patient education site
By a cyberfriend
TUMORS OF BLOOD VESSELS
Hemangiomas
Mostly hamartomas. You'll see a variety of these clinically.
* The endothelial cells are of course clonal and show some enhanced responses
to some growth factors
(J. Clin. Inv. 107: 745, 2001).
Capillary hemangiomas (little vessels) and cavernous hemangiomas (big vessels "resembling erectile
tissue") are common on the skin. Stork bites (backs of the neck and/or forehead of a baby)
usually involute (i.e., thrombose and organize) after a
few years, while cherry angiomas of the skin start popping up after age 20 or so.
{05888} hemangioma
{12235} hemangioma
{13041} hemangioma
{13042} hemangioma
{13044} hemangioma
{13045} hemangioma
{13047} hemangioma
{13048} hemangioma
{13050} hemangioma
{13051} hemangioma
{13141} hemangioma
{17507} hemangioma in liver
{21832} hemangioma
{21834} hemangioma
{21835} hemangioma
{22116} hemangioma
{22118} hemangioma
{22119} hemangioma
Port-wine stain (one form of "nevus flammeus"), fashionable in the Gorbachev era, can be treated by
laser if the patient wishes. A hemangioma in the meninges (bad, shunts blood away),
generally with an overlying port-wine stain in the V1 area (or check the eyelids; Pediatrics 87: 323,
1991), is Sturge-Weber syndrome.
Lasering them off, with dye-pulses: NEJM 338 1028, 1998.
{53705} Sturge-Weber
Pyogenic granuloma (noted misnomer; neither pyogenic nor a granuloma) pops up the gums of
pregnant ladies, or the skin of anybody. Grossly, it looks like a rotten cherry and bleeds
very easily. Microscopically, it
looks like granulation tissue.
{13141} "pyogenic granuloma"
{12786} "pyogenic granuloma"
{12789} "pyogenic granuloma"
{12225} pyogenic granuloma
* Epithelioid hemangiomas are curious bumps of small
vessels surrounding a single large one; the connective tissue between
the vessels is packed with eosinophils.
* Papillary endothelial hyperplasia is just an unusual
way for a thrombus to organize. Endothelial cells make little papillae.
The lack of anaplasia distinguishes it from an angiosarcoma.
Large hemangiomas can consume a person's platelets, the serious Kasabach-Merritt syndrome (Am.
J. Clin. Path. 99: 628, 1993; a kid received * 6622 units of platelets over 19 months, a new record).
{12237} Kasabach-Merritt giant hemangioma
Klippel-Trenaunay syndrome" is a huge capillary hemangioma plus
enlargement-deformity, always from a somatic mutation (* gene VG5Q: Nature 427:
640, 2004). A single extremity (or perhaps more than one) is involved.
Mayo Clin. Proc. 73: 28, 1998.
 * Golfer Casey Martin is the best-known Klippel-Trenaunay patient. In 2001,
the US Supreme Court ruled he could ride in a cart despite the PGA's complaining
it would give in an unfair advantage.
* Golfer Casey Martin is the best-known Klippel-Trenaunay patient. In 2001,
the US Supreme Court ruled he could ride in a cart despite the PGA's complaining
it would give in an unfair advantage.
Von Hippel Lindau anti-oncogene deletion syndrome results from mutated VHL. It features the most
troublesome hemangiomas in all of medicine, as well as renal cell carcinoma.
Glomangiomas (glomus tumors)
Painful tumors of the smooth muscle of the vestigial human glomus organs, little thermoregulatory
left-overs from mammalian evolution and found in the fingertips, toes, and coccyx (the rat's tail is
the most familiar glomus).
{09017} glomus tumor
Telangiectasias
"Dilatations of the ends of little vessels".
Osler-Weber-Rendu telangiectasias ("hereditary hemorrhage telangiectasia") result from any of several autosomal dominant genes (* some,
but not all, patients lack a binder for transforming growth factor beta). Patients have little vascular
malformations connecting little arteries and little veins along their whole GI tract (often easiest to see on
the lips, of course), and often lots of other places. These are prone to bleed. Reviews NEJM 333:
918, 1995; NEJM 345: 325, 2001 (* many of these patients also have
"idiopathic pulmonary hypertension", also from faulty vascular development; depends on the allele).
The familiar "liver spider" is a centrally dilated artery supplying several little arterioles
that
blanch when the "spider's body" is pressed.
Cancers of the blood vessels
Arcane stuff. We confirm the diagnosis using immunostains for von Willebrand's factor, or by finding Weibel-Palade bodies in the
endothelium on electron microscopy.
Hemangioendotheliomas are low-grade cancers of endothelium. They makes little vessels. Leave
the diagnosis to the pathologists.
(Hem)angiosarcomas: A host of aggressive cancers. Best-known is epidemic hepatic angiosarcoma,
caused by exposure to vinyl chloride or "Thorotrast" contrast medium. At other sites, they often
follow therapeutic radiation.
Epithelioid angiosarcomas (epithelioid hemangioendotheliomas)
are common, and look like carcinomas.
Bizarre new variant: Arch. Pat. Lab. Med. 121: 980, 1997.
Angiosarcomas are treacherous, especially to pathologists, and often look
deceptively benign. There may
be little or no anaplasia. Any "hemangioma"
that isn't nicely circumscribed should raise the suspicion of angiosarcoma.
* Angiosarcoma review: Cancer 77: 2400, 1996.
{10863} hemangiosarcoma
{21065} angiosarcoma, breast
{40635} angiosarcoma
Hemangiopericytomas: Low-grade cancer of the pericytes. As you'd expect, the tumor cells interlace
with vessels, beautifully demonstrated in reticulin-stained preparations. Again, leave the diagnosis
to the pathologists.
{09484}* hemangiopericytoma. This is subtle.
{09486}* hemangiopericytoma
{09489} hemangiopericytoma, reticulin stain
{09490} hemangiopericytoma, reticulin stain
Bacillary angiomatosis is a curious proliferation of small
vessels with cells packed with Bartonella bacteria (cat scratch and trench fevers).
It first appeared in AIDS patients, and is cured with antibiotics.
Kaposi's "sarcoma": The business cell is endothelium, and it can spread and choke off the viscera.
The cause, of course, is herpes virus 8.
Classic American Kaposi's of the pre-AIDS era mostly involved the legs of older men, and seldom
caused major problems.
Epidemic non-AIDS related Kaposi's is a disease mostly affecting young men in
central Africa. It's
more aggressive than classic Kaposi's, but not so much as in AIDS-related Kaposi's.
Renal transplant patients are prone to yet another Kaposi's variant.
Lymphangiomas: Hamartomas. The best-known is "cystic hygroma" of the necks of babies.
{23443} lymphangioma
{13392} cystic hygroma
|
 Benign lymphangioendothelioma
Benign lymphangioendothelioma
Pittsburgh Pathology Cases
|
Lymphangiosarcomas: Cancers of the lymphatics, generally arising in lymphedema (i.e., after
mastectomy, called * "Stewart-Treves syndrome") or after exposure to radiation.
HIGH TECHNOLOGY
Lifestyle changes have done wonders in reducing morbidity from atherosclerosis.
In addition, we can be thankful for interventions that have saved lives and
relieved symptoms when atherosclerosis does occur.
Angioplasty is surely familiar to you.
Artificial arteries are often made of gore-tex, like the thermal
running suits. They usually re-endothelialize (form a "neointima")
for only a cm or two
from where they are attached to the natural arteries. The remaining lumen is
lined by a mix of clot and scar ("pseudointima"). It is surprising that thrombosis is not
a more common problem.
* After thirty years of "study" in the U.S., evidence that acupuncture
actually works for ANY disease of the cardiovascular system remains
conspicuous by its absence. The best available is that some hypertensives'
blood pressure drops some while they are actually in the acupuncturist's
office, only to return to their usual levels when the treatments are
over (Circulation 103: 2038, 2001). A massive new study at Harvard
(SHARP -- Stop Hypertension with the Acupuncture Research Program) has
been undertaken, using sham acupuncture for controls (Cont. Clin. Tri. 25:
76, 2004); I predict it will not publish positive results.
* "How many miles of blood vessels are there in a pound of fat?" People
write me about this every once in a while. Let's figure it out. Assume an
adipocyte is 50 microns across; it'll vary from 10-100 depending on how fat
the person is. The fatter you are, the less vascular is your fat, which is one
more reason that this whole inquiry is silly.
In a section of body fat, which I examine often enough under the microscope,
the capillary (there has to be at least one) that supplies each fat cell is not
usually visible, so I'll assume one per adipocyte.
Put a single capillary between each pair of fat cells and
that's about 20 capillaries per millimeter, or 500 capillaries per inch.
Assume a pound of fat is a cube 4" on a side, which is good enough
for junk science, and that is 2000 capillaries
crosswise, for a total of 8000 inches.
Multiply by three for three dimensions, and this is 24,000 inches or ... well,
go figure. That this questions is fundamentally wrong-headed can be understood
by anyone who considers whether moving a certain total number of cars through Kansas City would be easier
with more highways or fewer highways. Further, the vast majority of these capillaries
are completely closed at any moment during your life, and not carrying
any blood. The real question isn't, "How many extra miles of blood vessels?",
but "How much rougher is it on my heart to be fat?" Think about walking around
carrying 100 lb of weights everywhere you go. The truth is that "education"
and moral exhortation do not cause people to lose weight; overeating is
programmed just like scratching when you itch.
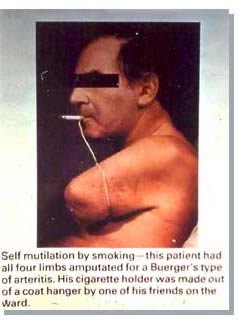 * SLICE OF LIFE REVIEW: VESSELS AND HEART
* SLICE OF LIFE REVIEW: VESSELS AND HEART
{03184} tricuspid valve, normal
{03187} tricuspid valve, normal
{03329} atrium, normal
{03344} hypertrophy & normal, (l) vent.
{03347} hypertrophy & normal, (l) vent.
{03401} comparison of atria, normal ra & la free walls
{03467} heart, normal histology
{03575} ventricular slice method of dissection normal heart
{03581} cardiac base method of dissection, normal heart
{03599} short axis dissection, normal heart
{03605} four chamber dissection, normal heart
{03611} long axis dissection, normal heart
{03629} cardiomyopathy, dilated; normal
{03683} pericardium intact opened, normal
{03686} pericardium opened removed, normal
{03689} pericardial sac, normal with and without heart removed
{03692} pericardium, normal with anterior portion removed
{03698} heart anterior, normal
{03716} heart, normal (r) (l) ant. oblique
{03719} heart anterior, normal
{03734} heart, normal (r)
{03749} heart, normal
{03758} tricuspid valve, normal
{03764} tricuspid valve (r) ventricle view, normal
{03767} mitral valve opened, normal
{03776} mitral chordae, normal
{03779} mitral valve, normal viewed from LA and LV aspects
{03785} aortic-mitral valvular continuity, normal
{03788} tricuspid mitral valves, normal comparison of shapes
{03791} tricuspid mitral valves, normal
{03794} heart, normal
{03797} heart, normal right ventricle
{03800} heart, normal left ventricle
{03803} heart, normal compare ventricle thick.
{03806} heart, normal
{03809} heart, normal
{03812} heart, normal
{03815} heart, normal: how to cut
{03818} heart, normal: how to cut
{03821} heart, normal: how to cut
{03851} myocardial cell, normal left ventricle
{03854} membranous septum (l) ventricle, normal
{03857} membranous septum (r) ventricle, normal
{03863} pulmonary valve, normal
{03866} aortic valve, normal
{03869} aortic valve closed opened, normal
{03872} aortic valve cusp in elderly, normal
{03881} aortic valve from above, normal
{03884} cardiac valves (all four), normal
{03899} coronary ostia, normal
{03902} aortic valve coronary ostia, normal
{03905} aortic valve coronary ostia, normal
{03908} coronary arteries, normal
{03911} coronary arteries sup. inf., normal
{03914} coronary artery dominance, normal
{03920} septum perforators of (l) ant. desc., normal
{03923} septum coronary arteries, normal
{03926} coronary arteries, normal
{03929} coronary arteries, normal
{04472} hear, normal
{04475} aorta, normal
{06218} superior vena cava aorta pulm. artery, normal
{06224} aortic arch, normal longitudinal section
{06233} vein, normal
{06539} coronary angiogram, normal
{09464} artery, normal
{09828} artery, normal
{11036} artery, normal
{11402} vertebral basilar artery, normal
{11405} vertebral basilar artery, normal
{11408} vertebral basilar artery, normal
{11738} heart, normal ventricle myocardium
{11799} heart, normal
{11800} heart, normal
{11809} aorta, intimal surface
{12889} venogram, normal
{12892} venogram, abnormal
{12894} venogram, abnormal
{14627} Purkinje fibers cross section
{14628} Purkinje fibers long.
{14687} capillary, normal
{14689} arteriole-venule, normal
{14692} artery, muscular
{14693} artery, muscular; shows internal elastic membrane
{14694} artery, small muscular
{14695} artery, small muscular
{14696} artery, muscular
{14697} artery, muscular; b=media, c=external elastic, d=adventitia, e=nerve
{14698} artery, vein
{14699} artery, vein
{14700} aorta, normal
{14701} aorta, normal (elastic stain)
{15047} adrenal medulla (central vein), normal
{15180} stomach, cardia
{15181} stomach, cardia
{15209} Purkinje fibers, heart
{15210} epicardium, #17
{15211} endocardium, #17
{15212} epicardium, #17
{15213} endocardium, #17
{15214} atrium, endocardium
{15215} atrium, endocardium
{15217} artery and vein, elastic stain
{15218} artery, #29
{15219} vein, #29
{15220} aorta, #22, elastic stain
{17466} artery, normal
{20234} ecg, normal
{20255} chest, normal x-ray
{20567} insufficiency, aortic with normal on r
{20798} vein
{20816} Purkinje fiber, heart
{20817} myocardium in cross section
{20818} epicardium with fat and blood vessel
{20819} myocardium with epicardium too
{20820} endocardium
{20821} atrium of heart, endocardial surface
{20822} atrium of heart, endocardial surface
{20823} atrium of heart, epicardial surface
{20824} artery and vein, longitudinal section
{20825} artery and vein, cross section
{20826} artery, elastic
{20839} artery
{31412} internal carotid artery, normal
{31442} straight sinus nerve vein of Galen, normal venous anatomy
{37643} heart, normal
{38015} artery, normal


|
|
Visitors to www.pathguy.com
reset Jan. 30, 2005: |
 Drop by
and meet Ed
Drop by
and meet Ed
Ed says, "This world would be a sorry place if
people like me who call ourselves Christians
didn't try to act as good as
other
good people
."
Prayer Request
 Teaching Pathology
Teaching Pathology

 Bone Marrow Embolus
Bone Marrow Embolus Congested liver, dead cells in zone 3
Congested liver, dead cells in zone 3 Great fibrin cap
Great fibrin cap Heart Failure Cells
Heart Failure Cells Hyalinized intramyocardial artery (diabetes)
Hyalinized intramyocardial artery (diabetes) Congested liver, live cells in zone 1
Congested liver, live cells in zone 1 Intrapulmonary hemorrhage
Intrapulmonary hemorrhage Myocardium
Myocardium Nodular diabetic glomerulosclerosis
Nodular diabetic glomerulosclerosis Myocardial ischemic scar
Myocardial ischemic scar Subendocardial ischemic scar
Subendocardial ischemic scar













 Cardiovascular Diseases
Cardiovascular Diseases
 OBJECTIVES: This is mastery material.
OBJECTIVES: This is mastery material.
 NORMAL ANATOMY
NORMAL ANATOMY
 BIRTH DEFECTS INVOLVING VESSELS
BIRTH DEFECTS INVOLVING VESSELS

 Mild, moderate & severe atherosclerosis
Mild, moderate & severe atherosclerosis 5.
Lack of exercise (made "official" in 1992), independent of the above (NEJM
330: 1565, 1992).
5.
Lack of exercise (made "official" in 1992), independent of the above (NEJM
330: 1565, 1992).
 Coronary graft vascular disease
Coronary graft vascular disease
 Buerger's disease ("thromboangiitis obliterans": review
Angiology 47: 419, 1996)
Buerger's disease ("thromboangiitis obliterans": review
Angiology 47: 419, 1996)

 Lymphedema
Lymphedema * Golfer Casey Martin is the best-known Klippel-Trenaunay patient. In 2001,
the US Supreme Court ruled he could ride in a cart despite the PGA's complaining
it would give in an unfair advantage.
* Golfer Casey Martin is the best-known Klippel-Trenaunay patient. In 2001,
the US Supreme Court ruled he could ride in a cart despite the PGA's complaining
it would give in an unfair advantage.
 Benign lymphangioendothelioma
Benign lymphangioendothelioma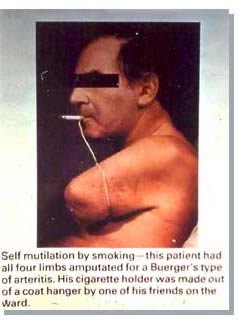 * SLICE OF LIFE REVIEW: VESSELS AND HEART
* SLICE OF LIFE REVIEW: VESSELS AND HEART



 Teaching Pathology
Teaching Pathology